Case StudyMembers Only
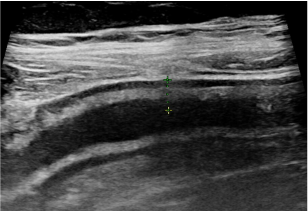
IUS Monthly: Acute Severe Ulcerative Colitis
IUS Monthly case highlighting the role of intestinal ultrasound in monitoring acute severe ulcerative colitis.
July 8, 2025
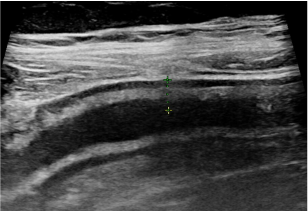
IUS Monthly case highlighting the role of intestinal ultrasound in monitoring acute severe ulcerative colitis.