Case StudyMembers Only
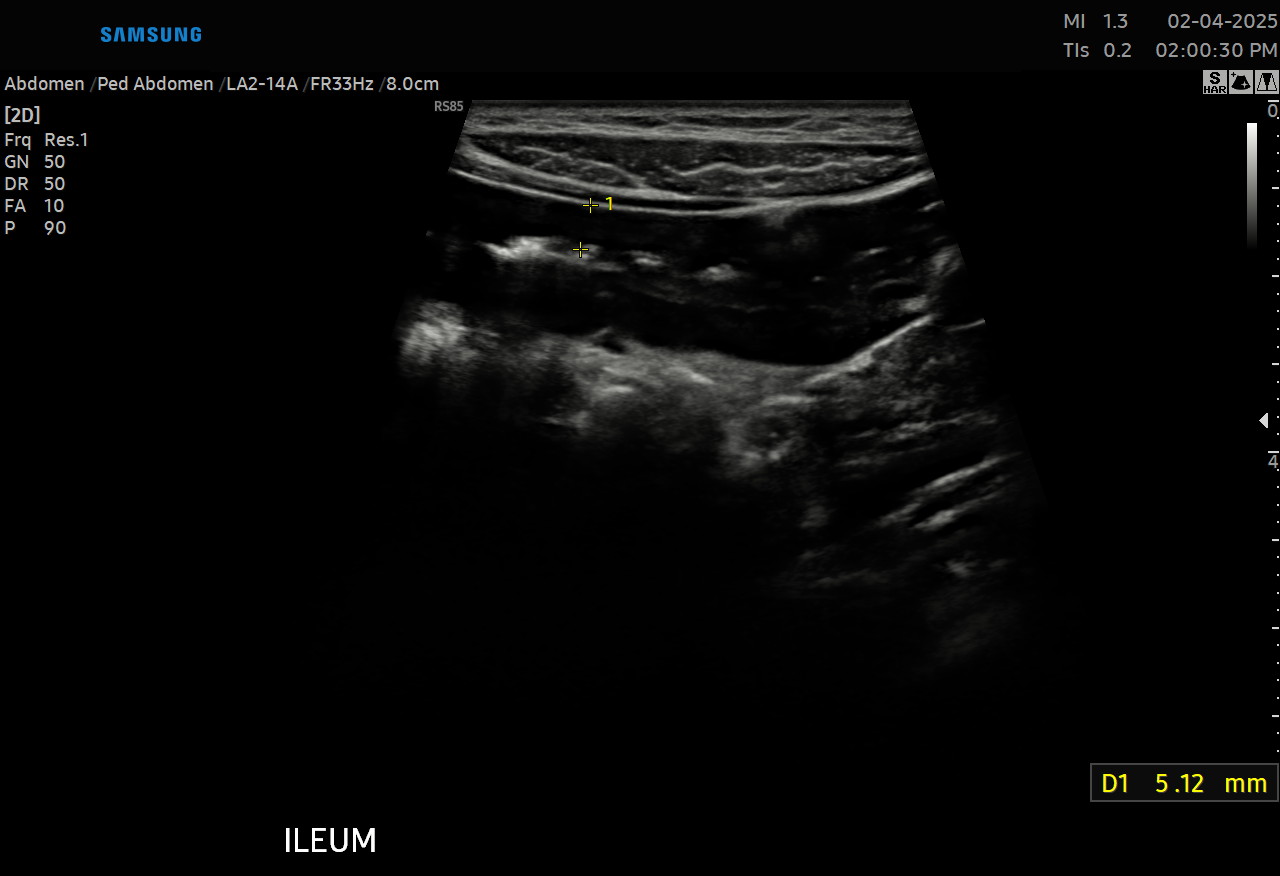
IUS Monthly: Pediatric Isolated Small Bowel Crohn's Disease
IUS Monthly case highlighting the role of intestinal ultrasound as a diagnostic screening tool in pediatric small bowel Crohn's disease.
July 8, 2025
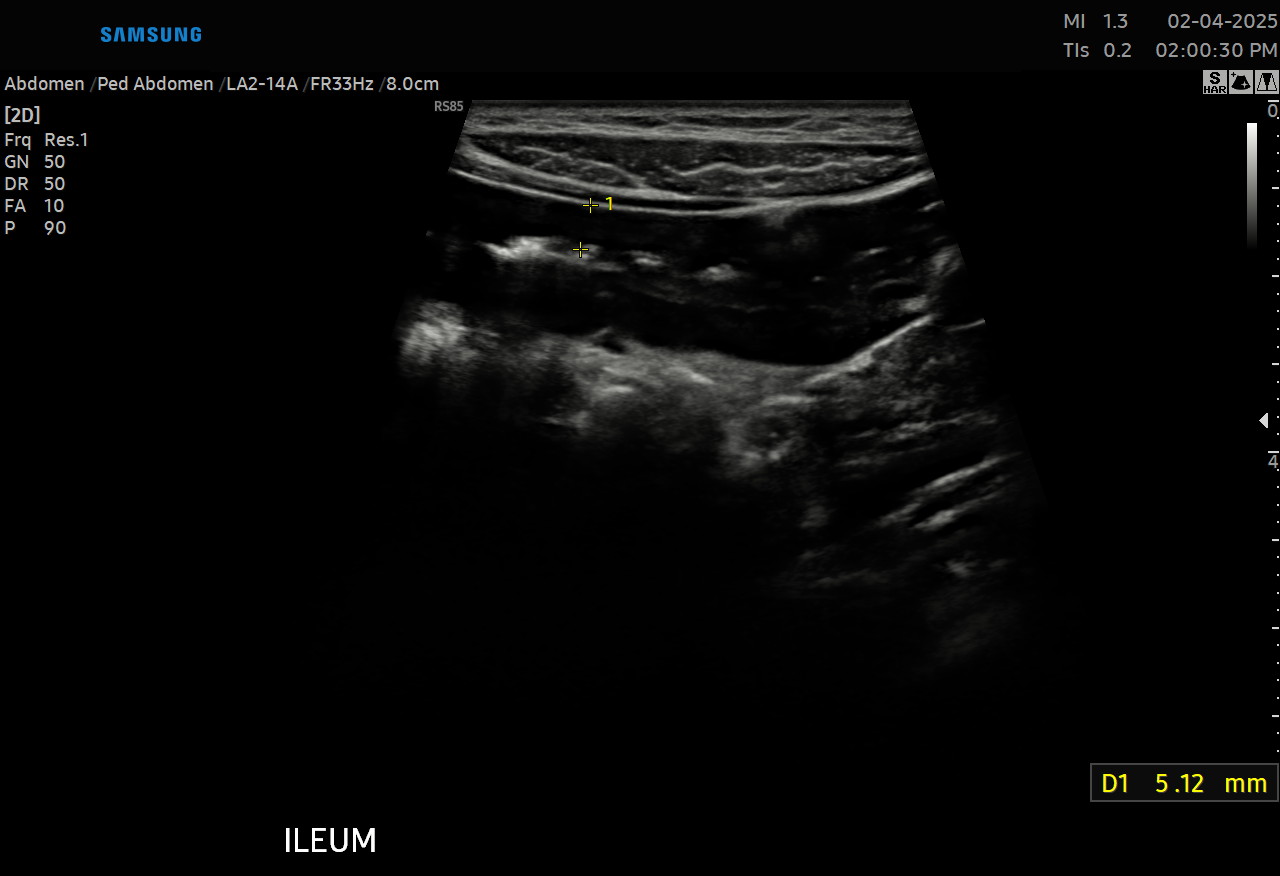
IUS Monthly case highlighting the role of intestinal ultrasound as a diagnostic screening tool in pediatric small bowel Crohn's disease.